Need PALS Certification?
It’s Trusted by Over 100,000+ Students
Register for PALS Certification
$119
Register for PALS Recertificaiton
$119
Welcome to the free PALS algorithm and guidelines offered by United Medical Education. Here you can prepare for your PALS certification exam and learn life saving interventions. Build your free student account to access our full training library.
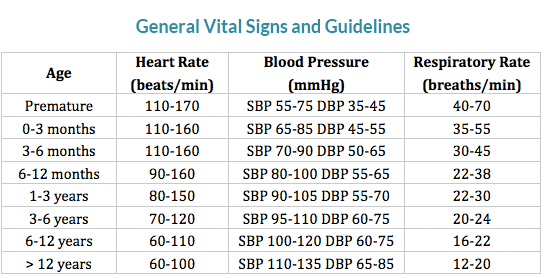
PALS Guidelines for Hypotension
- Neonate (0 to 28 days old): SPB < 60 mmHg
- Infants (1month to 12 montsh): SBP < 70 mmHg
- Children (1yr to 10yrs): SBP < 70+(2xage in years) mmHg
- Children (over 10yrs): SBP
These blood pressures defining hypotension commonly overlap with the lower normal SBP value spectrum.
Hemodynamics
It is important to be able to categorize your patients by their hemodynamic stability when choosing an appropriate treatment regimen.
Stable:
- Patient presents with an arrhythmia.
- Vital signs maintain patient asymptomatic without chest pain, shortness of breath, or confusion.
- Patient remains conscious.
- There is a high risk for patient becoming unstable.
Unstable:
- Patient presents with an arrhythmia.
- Vital signs cause patient to become symptomatic with chest pain, shortness of breath, or confusion.
- Patient has a high risk of death.
Dead:
- Patient presents with an arrhythmia.
- Patient has no pulse, is without vital signs, and/or is unconscious.
- Best chance for success is Electrical Therapy within 10 minutes of event!
ABG (Normal):
pH: 7.35-7.45
PaO2: 80-100 mmHg
PaCO2: 35-45 mmHg
HCO3: 22-26 mEq/L
O2 sat: 95-100% (on room air)
BE +/- 1
Lowest acceptable SBP for patients older than 1 yr = 70+ (2 x age in years)
Cardiac arrest in the pediatric patient is also commonly due to progressive shock. Compensated shock can be detected by evaluating the patient’s heart rate, presence of peripheral pulses, intravascular volume status, and end-organ perfusion. Sustained tachycardia can be a sign of early cardiovascular compromise. Bradycardia is a common sign of advanced shock and is frequently associated with hypotension.
Basic Treatment Associated with Stability
Stable:
O: Oxygen
M: Monitor
V: vascular access
Unstable & Dead:
I: IV access
C: CPR
E: ET intubation
D: Defibrillator/monitor
Secondary ABCD (Airway, Breathing, Circulation, Differential Diagnosis)
Airway (Two Providers)
- Initially provide rescue breaths using an ambu bag and a mask at full flow oxygen.
- Perform continued assessment of airway patency while giving breaths. (Condensation on mask during exhalation, chest rise, Et CO2)
- Have the person doing chest compressions pause during the 2 rescue breaths.


If the patient is not ventilating well or if there is a presumed risk of aspiration, insert an advanced airway device when prudent:
Endotreacheal Intubation is the preferred method.
(View the advanced airway section)
Breathing
Confirm correct placement of the advanced airway device:
- Look for condensation during exhalation.
- Look for equal bilateral chest rise.
- Confirming equal bilateral breath sounds with auscultation.
- Auscultate stomach to assure esophageal intubation didn’t occur.
- End-tidal CO2 should be verified during exhalation using monitor or ETD
- Use portable chest x-ray.
If incorrect placement:
- Remove the airway device, ventilate the patient using the ambu bag for a short period of time, and then reattempt placement.
If correct placement:
- Secure placement of the airway device.
Continue to monitor:
- oxygenation saturation with pulse oximeter
- end-tidal CO2
Rescue breathing during CPR with an advanced airway:
- 12-20 breaths per minute
- Chest compressions should be given continuously at a rate of 100 to 120 per minute.
Circulation
- Obtain IV or IO access.
- Monitors (ECG, BP cuff, pulse oximeter, et CO2 monitor)
Identify:
- heart rhythm
- Obtain a 12 lead ECG if possible.
- Initiate therapy of PALS algorithm corresponding with the identified heart rhythm. (Drug therapy, Electrical therapy, Pacing, etc.)
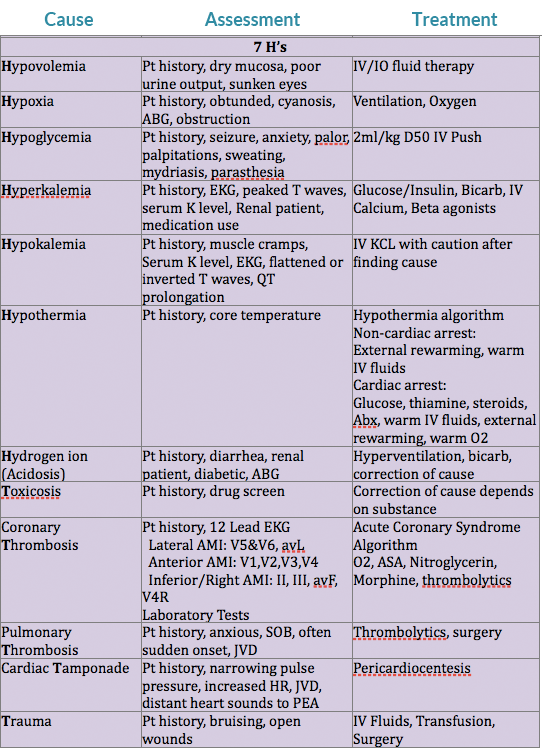
Differential Diagnosis
(needed for successful treatment of some patients)
Consider reversible causes of rhythm/arrhythmia.
Differential Diagnosis Chart:
Airway & Breathing
There are two important principles when evaluating the airway and breathing. First, is the airway patent or obstructed. Second, is there possible injury or trauma that would change the providers method of treating an obstructed airway or inefficient breathing.
Patent/obstructed
If the airway is patent there should be noticeable chest rise/expansion with either spontaneous respirations or with rescue breaths. The provider may also be able to hear or feel the movement of air from the patient.
A completely obstructed airway will be silent. An awake patient will lose their ability to speak, while both a conscious or unconscious patient will not have breath sounds on evaluation. If the patient is attempting spontaneous breaths without success, there may be noticeable effort of intercostal muscles, diaphram, or other accessory muscles without significant chest rise/expansion. The provider will also not feel or hear the movement of air. If the airway is partially obstructed snoring or stridor may be heard.
Cervical Spine Injury?
If the provider evaluates the patient to have an obstructed airway, intervention should take place. If the adverse event of the patient was witnessed and there is no reason to suspect a cercival spine injury, the provider should use the head tilt-chin lift maneuver to open the airway.
If there is a reason to suspect a cervical spine injury, if the patient’s adverse event went unwitnessed, if trauma occured, or the patient suffered drowning the jaw-thrust maneuver should be used to open the airway. If the jaw-thrust proves unsuccessful in opening the patient’s airway attempt an oropharangeal or nasopharangeal airway. If neither technique works, attempt an advanced airway using inline stabilization.
Brain Injury?
The breathing center that controls respirations is found within the pons and medulla of the brain stem. If trauma, hypoxia, stroke, or any other form of injury affects this area, changes in respiratory function may occur. Some possible changes are apnea (cessation of breathing), irregular breathing patterns, or poor inspiratory volumes. If the breathing pattern or inspiratory volumes are inadequate to sustain life, rescue breathing will be required, and an advanced airway should be placed.
Oral Airway:
- Assure the artificial airway is the appropriate size for the patient.
- The airway should be easily inserted with a tongue blade.
- Avoid use in patients with an active gag reflex.
Nasal Trumpet Airway:
- Best practice is to lube before insertion.
- Careful not to cause trauma to nasal mucosa (results in bleeding).
- This is reasonably tolerated by patients with an active gag reflex.
Advanced Airways
Indications:
- When you are unable to open airway using head tilt-chin lift or jaw thrust maneuvers.
- If you have difficulty forming a seal with the face mask.
- If the patient requiring continued ventilatory support.
- When the patient has a high risk for aspiration (provide an ETT or Combitube).
Remember, a patient should be unconscious or sedated without an active gag reflex before instrumentation of the airway occurs with an ETT, Combitube, or LMA.
Endotracheal Tube (ETT)
- Requires additional instrument for insertion (laryngoscope, glidescope, fiberoptic).
- Laryngoscope blades (average adult size): MAC 3 or 4, Miller 2 or 3
- Same sized laryngoscopes or smaller sizes can be used for pediatrics.
- ETTs require mastery of technique for consistent appropriate placement.
Average size of ETT for orotracheal intubation (mm):
- Uncuffed: tube = (age/4)+4
- Cuffed: tube = (age/4)+3
1) The ETT is placed into the trachea, having direct visualization of the vocal cords.
- Children over 1 year: Depth of intubation (cm) = age/2+13
- Children under 1 year: Depth of intubation (cm) = weight/2+8
2) Tracheal cuff of the ETT is then inflated.
- Allows for positive pressure ventilation.
- Reduces risk of aspiration.
- Helps maintain placement of ETT.
3) Confirm placement of ETT.
4) Secure the ETT in place.



Laryngeal Mask Airway (LMA)
Visualization of the vocal cords is not required for insertion.
- When inserting the LMA have the laryngeal cuff deflated.
- Guide in the LMA cuff without folding back the tip, pressing it against the hard palate.
- Advance the LMA till the cuff lies in the pharynx.
- After placement, inflate the laryngeal cuff and check for an adequate seal by using positive pressure ventilation.
Positive pressure ventilation is generally kept under 20 CmH2O to prevent inflation of the stomach.
The patient is still at high risk of aspiration, even with an appropriately placed LMA.
Cardiac/Electrical Therapy
Transcutaneous Pacemaker (External Pacemaker):
Used to treat unstable bradycardias not responding to drug therapy. Provides temporary pacing through the skin in emergency situations.
- Place pads and electrodes in correct position to assure an appropriate ECG reading.
- Set the pacer 10-20 beats per min above the patient’s intrinsic heart rate or 60 beats per min if there is no intrinsic heart rate.
- Start at O mA and work energy level up until you have capture (heart pulsation).
- Assure the patient is sedated and comfortable during pacer delivery.
Cardioversion:
- Used if drug therapy and vagal maneuvers fail.
- Used when patient has a pulse.
- Used to treat Atrial Fibrillation, Atrial Flutter, Atrial Tach, and Symptomatic VT.
- Shock performed at peak of R wave.
- Requires proper lead/pad placement to monitor ECG.
Pediatric shock energy level:
Monophasic or Biphasic: 0.5-1.0 J/kg
Assure the patient is sedated and comfortable during shock delivery.
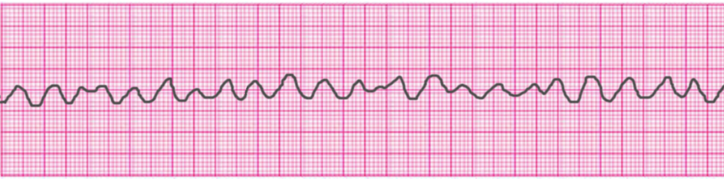
Defibrilation:
- Used to treat VF and pulseless VT.
- Delivery within first 5 mins of cardiac arrest has best results.
- CPR before and after each shock improves outcomes.
Pediatric shock energy level:
Monophasic or Biphasic: 2 J/kg for the first attempt and 4 J/kg for subsequent attempts.

Common Cardiac Rhythms
Normal Sinus Rhythm

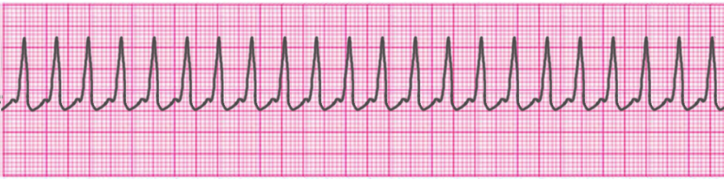
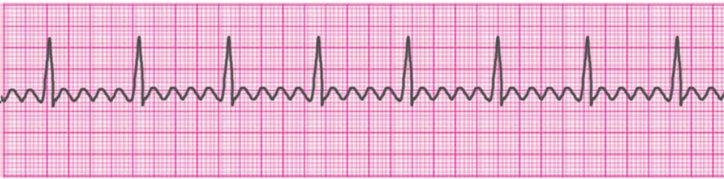
Atrial Tachycardia

Supraventricular Tachycardia
Atrial Fibrillation

Atrial Flutter
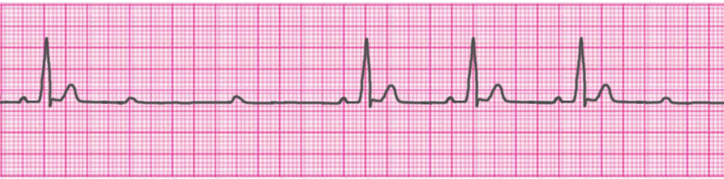
Sinus Bradycardia

1° Atrioventricular Block

2° Atrioventricular Block- Type 1 (Mobitz I/Wenckebach)
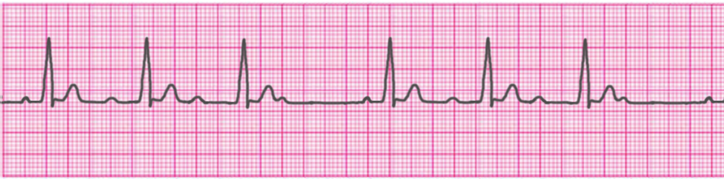
2° Atrioventricular Block- Type 2 (Mobitz II/Hay)
3° Atrioventricular Block (Complete Heart Block)
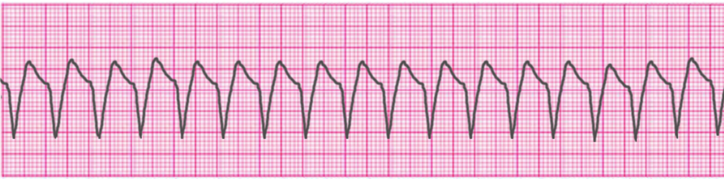
Ventricular Tachycardia – Monomorphic
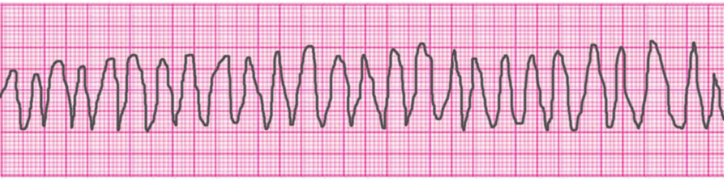
Ventricular Tachycardia – Polymorphic
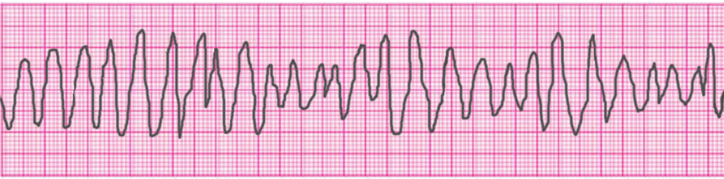
Ventricular Tachycardia – Torsades de Pointes
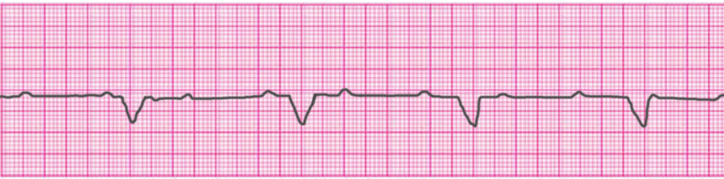
Ventricular Fibrillation
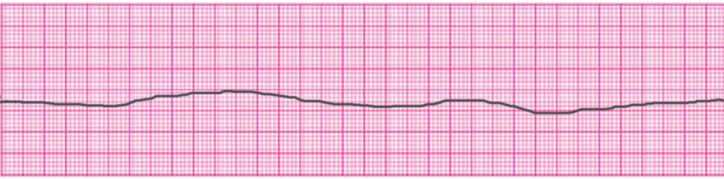
Asystole
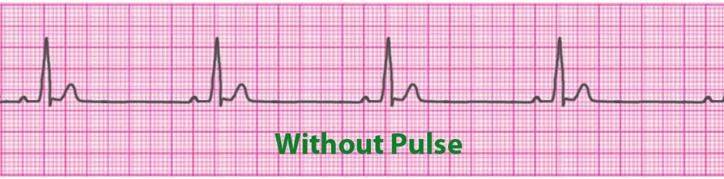
Pulseless Electrical Activity (PEA)
Access Our Complete Training Materials.
Lets Get You Certified!
Register for PALS Certification
$119
Register for PALS Recertificaiton
$119
Cardiopulmonary Resuscitation at Birth
- Dry and warm the infant
- Position the infant supine on a hard flat surface in sniffing position
- Suction and stimulate the infant
- Provide oxygen therapy, IV/IO
- Monitors: SpO2, BP, ECG
If HR < 100 BPM:
- Assess and provide ventilation support.
If HR < 60 BPM:
- Provide chest compressions with concurrent ventilation support.
- If patient fails to respond to stimulus and treatment: Assess rhythm and provide appropriate drug treatment.
Tachycardias
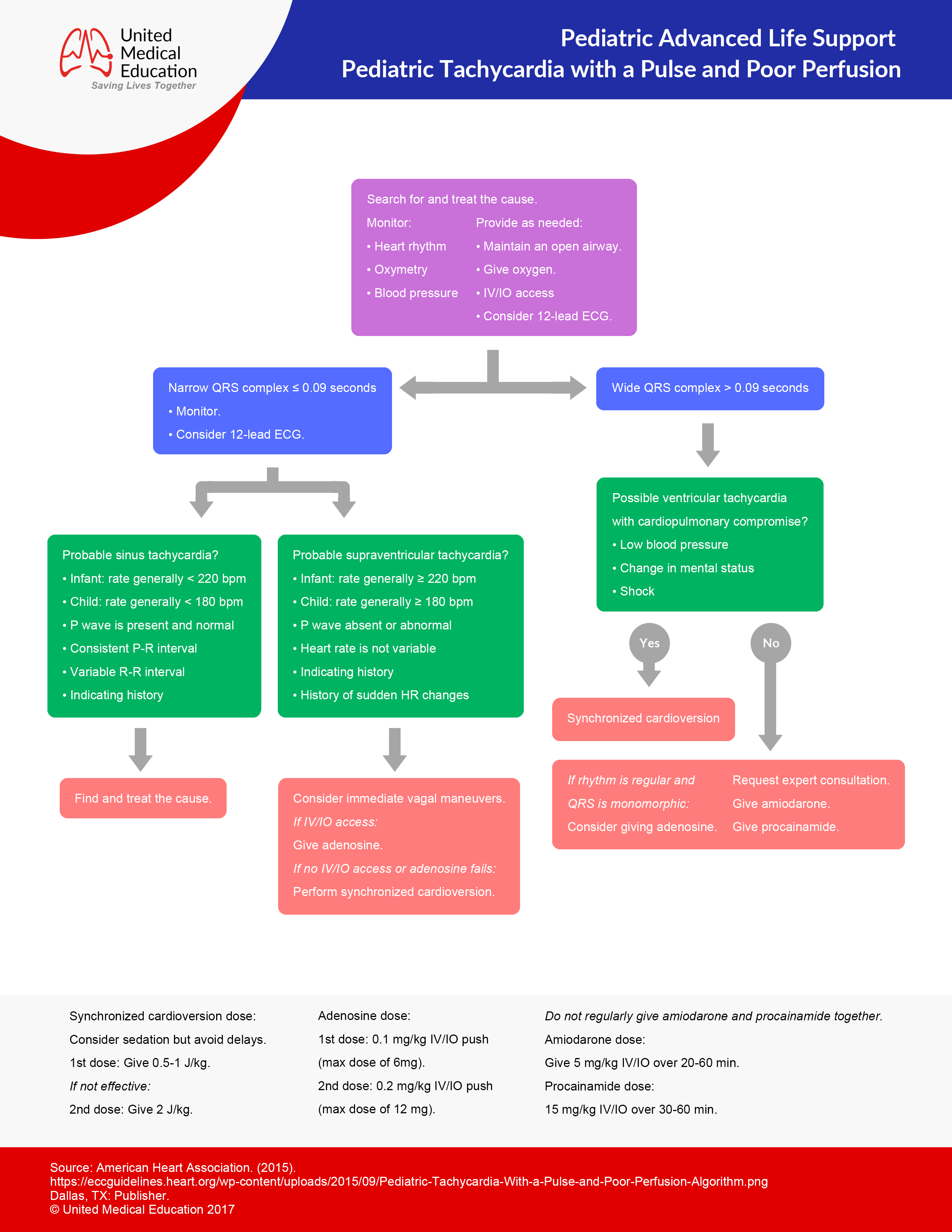
- Begin CABD
- Monitors: SpO2, BP, ECG
- Provide oxygen therapy, IV or IO.
- Assess rhythm and possible cause.
Narrow QRS Complex
Sinus Tachycardia
Treat reversible causes:
- Hypoxia
- Acidosis
- Pulmonary thrombosis
- Tension pneumothorax
- Coronary thrombosis
- Cardiac tamponade
- Hypoglycemia
- Hyperkalemia
- Hypokalemia
- Hypothermia
- Hypovolemia
- Poisoning
SupraVentricular Tachycardia (SVT)
(infants: > 220 BPM; children: > 180 BPM)
Stable:
- Vagal maneuvers
- Adenosine: 0.1 mg/kg IVP or IOP (6mg maximum dose)
- May repeat: Adenosine 0.2 mg/kg IVP or IOP
- Sedation and synchronized cardioversion
- 1st Cardioversion: 0.5-1.0 J/kg
- Following Cardioversions: 2 J/kg
Unstable:
- Sedation and synchronized cardioversion
- 1st Cardioversion: 0.5-1.0 J/kg.
- Following Cardioversions: 2 J/kg
Wide QRS Complex
Ventricular Tachycardia with a pulse
stable:
If regular monomorphic:
- Adenosine: 0.1 mg/kg IVP or IOP (6mg maximum dose)
- Amiodarone: 5 mg/kg IV or IO in 20 to 60 minutes
- Procainamide: 15mg/kg IV or IO in 30 to 60 minutes
Unstable:
- Consider synchronized cardioversion
- 1st Cardioversion: 0.5-1.0 J/kg.
- Following Cardioversions: 2 J/kg
Pulseless Ventricular Tachycardia / Refractory Ventricular Fibrillation
Unstable (shock, severe hypotension)
Electrical therapy:
- Initiate electrical therapy as soon as possible!
- 1st Defibrillate: Defibrillate at 2j/kg
- If 1st Defibrillate unsuccessful: 2nd Defibrillate at 4j/kg
- If 2nd Defibrillate unsuccessful: following Defibrillations at 4 j/kg
Drug therapy:
- Give Epinephrine 1:10,000: 0.01 mg/kg by IV or IO (or give Epinephrine 1:1,000: 0.1 mg/kg by ET)
- Give Lidocaine: 1 mg/kg by IV or IO
- Give Amiodarone: 5mg/kg by IV or IO
Toursades de Pointe or Low Magnesium Level
- Give Magnesium: 25-50 mg/kg by IV or IO
Bradycardia (Rate < 60)
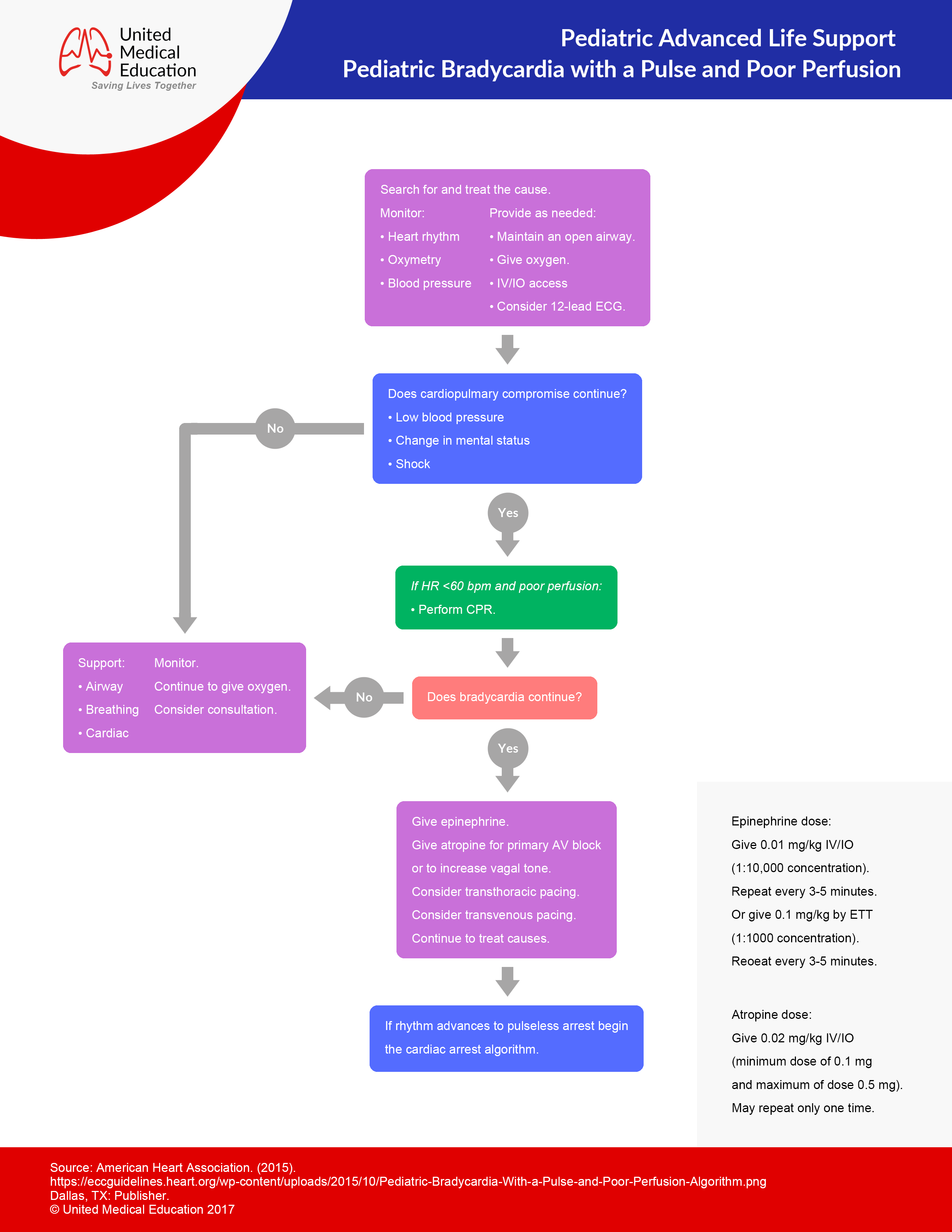
- Begin CABD
- Monitors: SpO2, BP, ECG
- Provide oxygen therapy, IV or IO
- Assess rhythm and possible cause (Most common cause is hypoxia)
- Treat possible causes with appropriate drug, electrolyte, and fluid therapy
- Place defibrillator on patient for possible electrical therapy.
Drug therapy:
- Give Epinephrine in a 1:10,000 solution: 0.01 mg/kg by IV or IO every 3 to 5 minutes (or give Epinephrine in a1:1,000 solution: 0.1mg/kg by ETT every 3 to 5 minutes)
- Atropine: 0.02 mg/kg by IV or IO with a minimum single dose of 0.1mg and a maximum single dose of 0.5mg in a child (used for AV block and to increase vagal tone).
Electrical therapy:
- Consider transcutaneous pacing
Asystole / Pulseless Electrical Activity (PEA)
- Begin CABD
- Monitors: SpO2, BP, ECG
- Provide oxygen therapy, IV
- Assess rhythm and possible cause
Treat reversible causes:
- Hypoxia
- Acidosis
- Pulmonary thrombosis
- Tension pneumothorax
- Coronary thrombosis
- Cardiac tamponade
- Hypoglycemia
- Hyperkalemia
- Hypokalemia
- Hypothermia
- Hypovolemia
- Poisoning
Drug therapy:
- Epinephrine in a 1:10,000 solution: 0.01 mg/kg by IV/IO every 3 to 5 minutes (or Epinephrine in a 1:1,000 solution: 0.1 mg/kg by ETT every 3 to 5 minutes)
Shock
- Assess for poor perfusion and altered mental status.
- Begin CABD
- Monitors: SpO2, BP, ECG
- Provide oxygen therapy, IV
- Assess rhythm and possible cause
- Labs: blood gas, lactate, glucose, CBC, ionized calcium, cultures.
- Provided repeated IV bolus’ of crystalloids at 20 ml/kg. (Cease bolus’ at indication of fluid in lungs showing repiratory distress or rales. Also, cease bolus’ if hepatomegaly presents.)
Additional interventions:
- Administer antibiotics STAT (for septic shock)
- Correct hypoglycemia
- Correct hypocalcemia
- Vasopressors
- Administer hydrocortisone if possible adrenal insufficiency.
If poor end-organ perfusion continues after fluid administration:
- Vasopressor therapy
- Titrate according to need (ScvO2 > 70%)
- Central line, arterial line may be indicated
- Warm Shock (vasodilated, hypotensive): administer Norepinephrine 0.1-2 mcg/kg/minute and titrate to BP
- Cold Shock (vasoconstricted, hypotensive): administer Epinephrine 0.1-1 mcg/kg/minute and titrate to BP
Normal BP with poor perfusion:
- administer dopamine 2-20 mcg/kg/minute
If ScvO2 >70% and hypotension:
Likely due to warm shock.
- Continue IV fluid therapy
- Continue administering Norepinephrine 0.1-2 mcg/kg/minute, titrate to BP
- Consider administering Vasopressin 0.2-2 milliunits/kg/minute
If ScvO2 <70% and normotension:
- Transfuse PRBC for a Hgb > 10g/dl
- Continue IV fluid therapy
- Attempt to optimize arterial oxygenation
- Consider administering Milrinone loading dose of 50mcg/kg over 10-60 minutes and then o.25-0.75 mcg/kg/min
- Consider administering Nitroprusside 0.3-1 mcg/kg/minute then titrate (maximum of 8 mcg/kg/minute)
- Consider administering Dobutamine 2-20 mcg/kg/minute
If ScvO2 <70% and hypotension:
Likely due to cold shock.
- Transfuse PRBC for a Hgb > 10g/dl
- Continue IV fluid therapy
- Attempt to optimize arterial oxygenation
- Continue administering Epinephrine 0.1-1 mcg/kg/minute and titrate to BP and end-organ perfusion
- Consider administering Dobutamine 2-20 mcg/kg/minute and titrate
- Consider administering Norepinephrine 0.1-2 mcg/kg/minute and titrate
Congratulations!
You’re Ready to Certify.
Register for PALS Certification
$119
Register for PALS Recertificaiton
$119
