Welcome to our ACLS algorithms and guidelines page offered free here at United Medical Education. Take your time to review each section. Here you’ll find everything you’ll need to prepare for ACLS certification. We have a separate page for additional information on the anatomy of the human heart.
Introduction: What is Advanced Cardiac Life Support (ACLS)?
ACLS is an acronym that stands for Advanced Cardiac Life support. ACLS teaches healthcare professionals advanced interventional protocols and algorithms for the treatment of cardiopulmonary emergencies. These include primary survey, secondary survey, advanced airways, myocardial infarction, cardiac arrest, tachycardias, bradycardias, and stroke. The treatment protocols have been established through collaborative clinical research and later published by the International Liaison Committee on Resuscitation (ILCOR).
Need ACLS Certification?
It’s Trusted by Over 100,000+ Students
Register for ACLS Certification
$119
Register for ACLS Recertificaiton
$119
Secondary ABCD (Airway, Breathing, Circulation, Differential Diagnosis)
Airway (two provider)
- Initially provide rescue breaths using an ambu bag and a mask at full flow oxygen.
- Perform continued assessment of airway patency while giving breaths.
- Have the person doing chest compressions pause during the 2 rescue breaths.


If the patient is not ventilating well or if there is a presumed risk of aspiration, insert an advanced airway device when prudent:
Endotreacheal Intubation is the preferred method.
(View the advanced airway section)
Breathing
Confirm correct placement of the advanced airway device:
- Look for condensation during exhalation.
- Look for equal bilateral chest rise.
- Confirming equal bilateral breath sounds with auscultation.
- Auscultate stomach to assure esophageal intubation didn’t occur.
- End-tidal CO2 should be verified during exhalation using monitor or ETD
- Use portable chest x-ray.
If incorrect placement:
- Remove the airway device, ventilate the patient using the ambu bag for a short period of time, and then reattempt placement.
If correct placement:
- Secure placement of the airway device.
Continue to monitor:
- oxygenation saturation with pulse oximeter
- end-tidal CO2
Rescue breathing during CPR with an advanced airway:
- 8-10 breaths per minute (1 breath every 6-8 seconds)
- Chest compressions should be given continuously at a rate of 100 to 120 per minute.
Circulation
- Obtain IV or IO access.
- Monitors (ECG, BP cuff, pulse oximeter, et CO2 monitor)
Identify:
- heart rhythm
- Obtain a 12 lead ECG if possible.
- Initiate therapy of ACLS algorithm corresponding with the identified heart rhythm. (Drug therapy, Electrical therapy, Pacing, etc.)
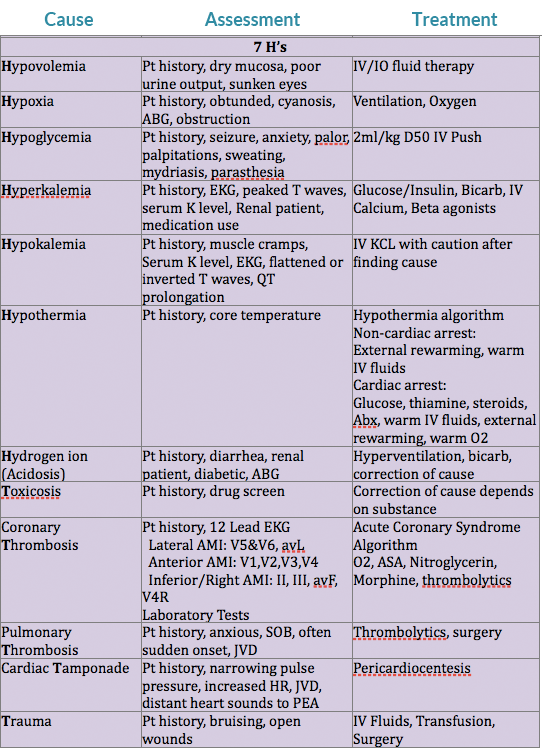
Differential Diagnosis
(needed for successful treatment of some patients)
Consider reversible causes of rhythm/arrhythmia.
Differential Diagnosis Chart:
Airway & Breathing
There are two important principles when evaluating the airway and breathing. First, is the airway patent or obstructed. Second, is there possible injury or trauma that would change the providers method of treating an obstructed airway or inefficient breathing.
Patent/obstructed
If the airway is patent there should be noticeable chest rise/expansion with either spontaneous respirations or with rescue breaths. The provider may also be able to hear or feel the movement of air from the patient.
A completely obstructed airway will be silent. An awake patient will lose their ability to speak, while both a conscious or unconscious patient will not have breath sounds on evaluation. If the patient is attempting spontaneous breaths without success, there may be noticeable effort of intercostal muscles, diaphram, or other accessory muscles without significant chest rise/expansion. The provider will also not feel or hear the movement of air. If the airway is partially obstructed snoring or stridor may be heard.
Cervical Spine Injury?
If the provider evaluates the patient to have an obstructed airway, intervention should take place. If the adverse event of the patient was witnessed and there is no reason to suspect a cercival spine injury, the provider should use the head tilt-chin lift maneuver to open the airway.
If there is a reason to suspect a cervical spine injury, if the patient’s adverse event went unwitnessed, if trauma occured, or the patient suffered drowning the jaw-thrust maneuver should be used to open the airway. If the jaw-thrust proves unsuccessful in opening the patient’s airway attempt an oropharangeal or nasopharangeal airway. If neither technique works, attempt an advanced airway using inline stabilization.
Brain Injury?
The breathing center that controls respirations is found within the pons and medulla of the brain stem. If trauma, hypoxia, stroke, or any other form of injury affects this area, changes in respiratory function may occur. Some possible changes are apnea (cessation of breathing), irregular breathing patterns, or poor inspiratory volumes. If the breathing pattern or inspiratory volumes are inadequate to sustain life, rescue breathing will be required, and an advanced airway should be placed.
Oral Airway:
- Assure the artificial airway is the appropriate size for the patient.
- The airway should be easily inserted with a tongue blade.
- Avoid use in patients with an active gag reflex.
Nasal Trumpet Airway:
- Best practice is to lube before insertion.
- Careful not to cause trauma to nasal mucosa (results in bleeding).
- This is reasonably tolerated by patients with an active gag reflex.
Advanced Airways
Indications:
- When you are unable to open airway using head tilt-chin lift or jaw thrust maneuvers.
- If you have difficulty forming a seal with the face mask.
- If the patient requiring continued ventilatory support.
- When the patient has a high risk for aspiration (provide an ETT or Combitube).
Remember, a patient should be unconscious or sedated without an active gag reflex before instrumentation of the airway occurs with an ETT, Combitube, or LMA.
Endotracheal Tube (ETT)
- Requires additional instrument for insertion (laryngoscope, glidescope, fiberoptic).
- Laryngoscope blades (average adult size): MAC 3 or 4, Miller 2 or 3. ETTs require mastery of technique for consistent appropriate placement.
- Average size of ETT for orotracheal intubation for adults is 7.5mm.
- The ETT is placed into the trachea, having direct visualization of the vocal cords.
Average depth of intubation:
- adult male is 23cm
- adult female is 21cm
- Tracheal cuff of the ETT is then inflated.
- Allows for positive pressure ventilation.
- Reduces risk of aspiration.
- Helps maintain placement of ETT.
- Confirm placement of ETT.
- Secure in place of ETT.



Esophageal-Tracheal Combitube
- Gently advance the combitube into the mouth midline along the base of the tongue.
- Assure tube rotation of the combitube is following the curvature of the pharynx.
- Cease advancement of the tube once the heavy black rings reach the patient’s teeth.
- The Combitube is blindly placed into the esophagus 80% of the time and into the trachea 20% of the time.
- The combitube provides ventilatory access irregardless of tracheal or esophageal intubation.
- Inflate the pharangeal cuff with 100ml of air. Prevents leak through the nose and mouth. Helps secure placement.
- Inflate the tracheal cuff with 15ml of air. Prevents ventilation of stomach. Reduces risk of aspiration of stomach content.
- Secure in place of ETT.
First attempt confirmation of esophageal intubation by ventilating through the esophageal tube. (See “Secondary ABCD” section regarding placement confirmation)
If placement not confirmed through esophageal tube:
- Attempt confirmation of tracheal intubation by ventilating through the tracheal tube. (See “Secondary ABCD” section regarding placement confirmation)
Once placement has been confirmed:
- Mark which tube should be used for ventilation.
- Secure tube in place.
- Both cuffs must be inflated to appropriately ventilate a patient in the case of esophageal intubation.
Laryngeal Mask Airway (LMA)

Visualization of the vocal cords is not required for insertion.
- When inserting the LMA have the laryngeal cuff deflated.
- Guide in the LMA cuff without folding back the tip, pressing it against the hard palate.
- Advance the LMA till the cuff lies in the pharynx.
- After placement, inflate the laryngeal cuff and check for an adequate seal by using positive pressure ventilation.
Positive pressure ventilation is generally kept under 20 CmH2O to prevent inflation of the stomach. LMA’s are contraindicated for the morbidly obese patient.
The patient is still at high risk of aspiration, even with an appropriately placed LMA. LMA’s are contraindicated in patients with GERD, full stomachs, and pregnant women.
Cardiac/Electrical Therapy
Transcutaneous Pacemaker (External Pacemaker):
Used to treat unstable bradycardias not responding to drug therapy. Provides temporary pacing through the skin in emergency situations.
- Place pads and electrodes in correct position to assure an appropriate ECG reading.
- Set the pacer 10-20 beats per min above the patient’s intrinsic heart rate or 60 beats per min if there is no intrinsic heart rate.
- Start at O mA and work energy level up until you have capture (heart pulsation).
- Assure the patient is sedated and comfortable during pacer delivery.
Cardioversion:
- Used if drug therapy and vagal maneuvers fail.
- Used when patient has a pulse.
- Used to treat Atrial Fibrillation, Atrial Flutter, Atrial Tach, and Symptomatic VT.
- Shock performed at peak of R wave.
- Requires proper lead/pad placement to monitor ECG.
Shock energy level:
Monophasic: 100-200J
Biphasic: factory recommendations (generally 100J)
Assure the patient is sedated and comfortable during shock delivery.
Defibrilation:
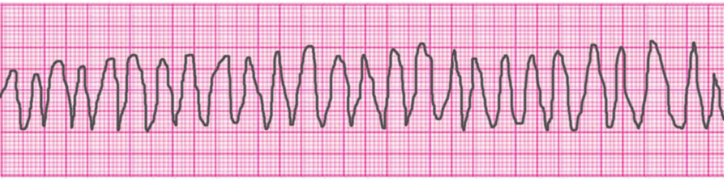
- Used to treat VF and pulseless VT.
- Delivery within first 5 mins of cardiac arrest has best results.
- CPR before and after each shock improves outcomes.
Shock energy level:
Monophasic: 360J
Biphasic: factory recommendations (generally 120-200J)

Common Cardiac Rhythms
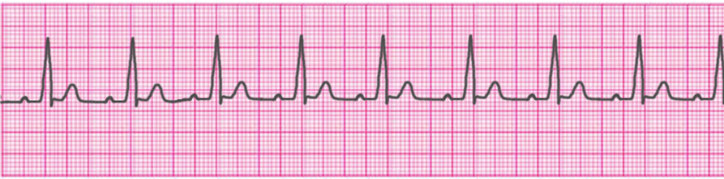
Normal Sinus Rhythm
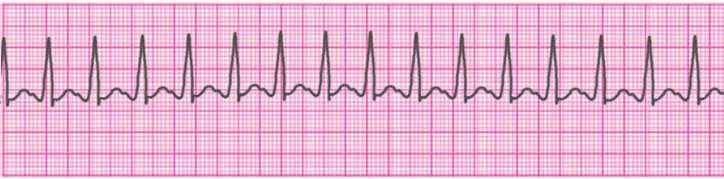
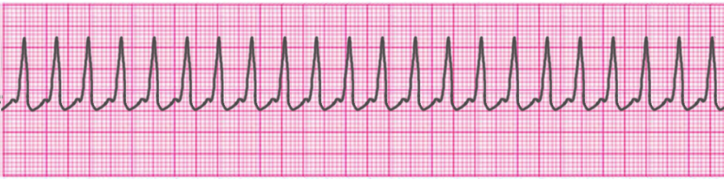
Atrial Tachycardia
Supraventricular Tachycardia
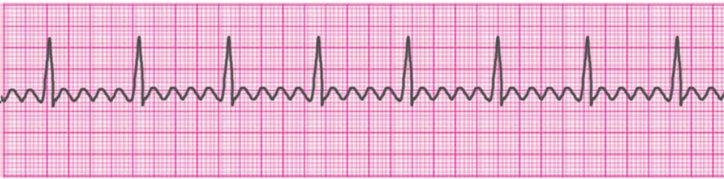
Atrial Fibrillation

Atrial Flutter
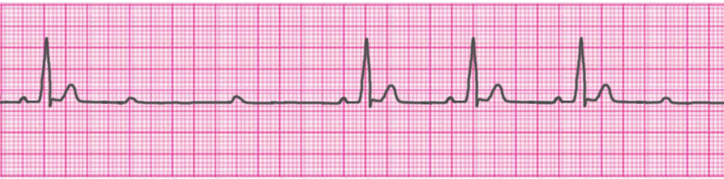
Sinus Bradycardia
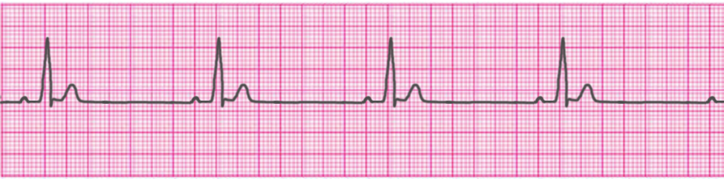
1° Atrioventricular Block

2° Atrioventricular Block- Type 1 (Mobitz I/Wenckebach)
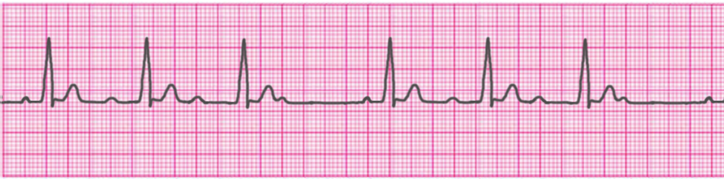
2° Atrioventricular Block- Type 2 (Mobitz II/Hay)
3° Atrioventricular Block (Complete Heart Block)

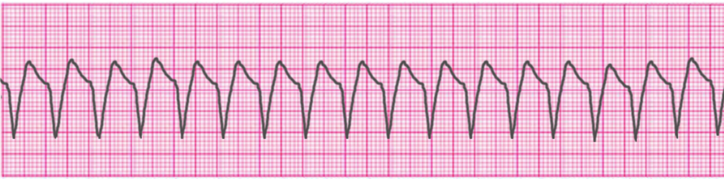
Ventricular Tachycardia – Monomorphic
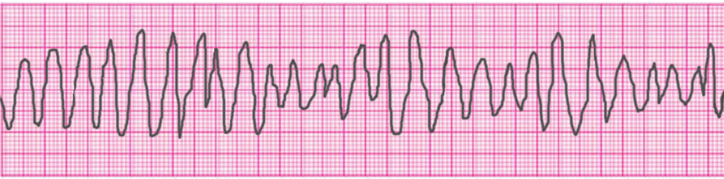
Ventricular Tachycardia – Polymorphic
Ventricular Tachycardia – Torsades de Pointes
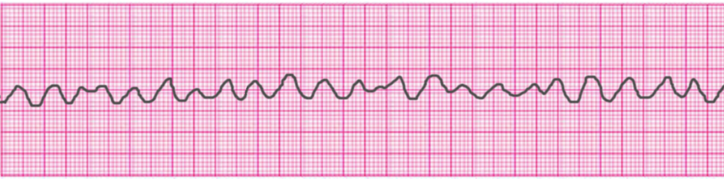
Ventricular Fibrillation
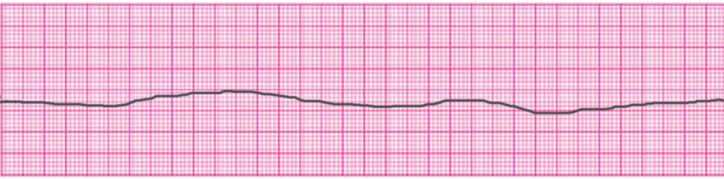
Asystole
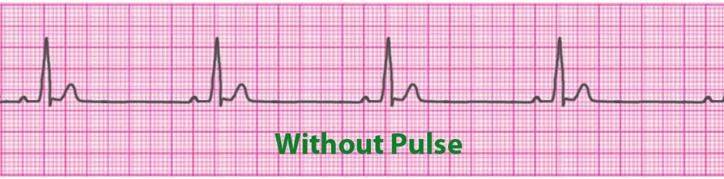
Pulseless Electrical Activity (PEA)
Access Our Complete Training Materials.
Lets Get You Certified!
Register for ACLS Certification
$119
Register for ACLS Recertificaiton
$119
Acute Myocardial Infarction
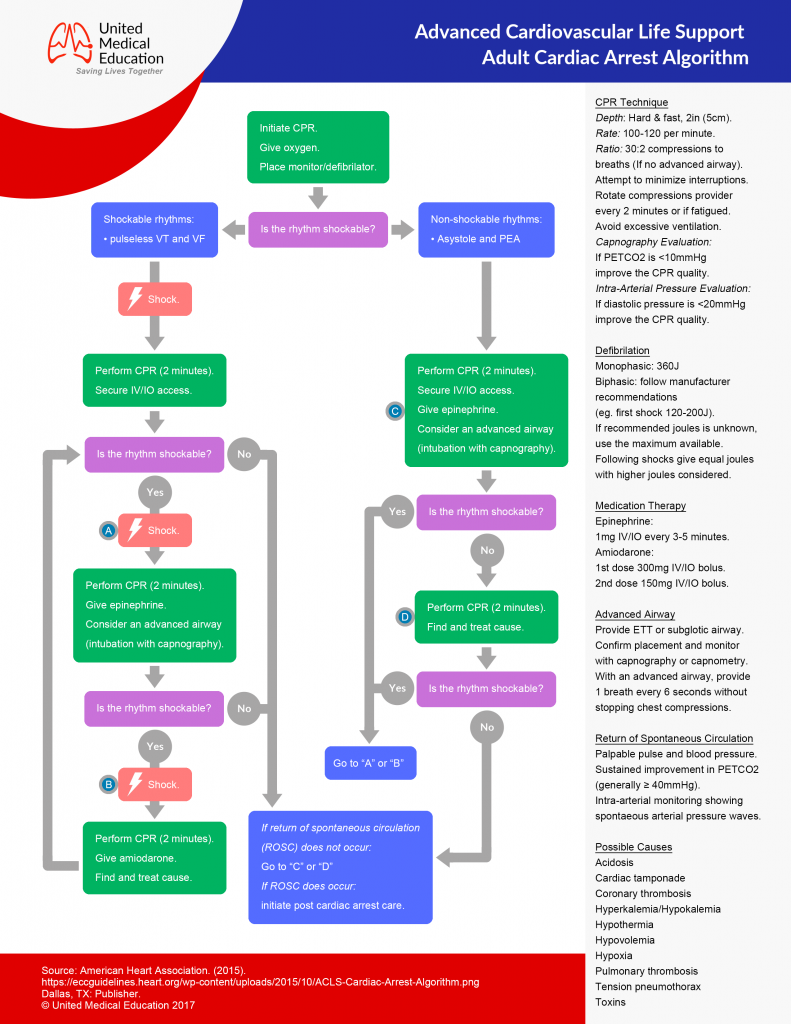
ACLS Adult Cardiac Arrest Algorithm
- Determine if the patient is Stable or Unstable.
- Initiate CABD and Secondary ABCD.
- Use appropriate ACLS algorithm.
- Generally accepted treatments: “MONA”: Morphine, Oxygen, Nitrates, and Aspirin
- Consider fibrinolytic therapy.
Tachycardias
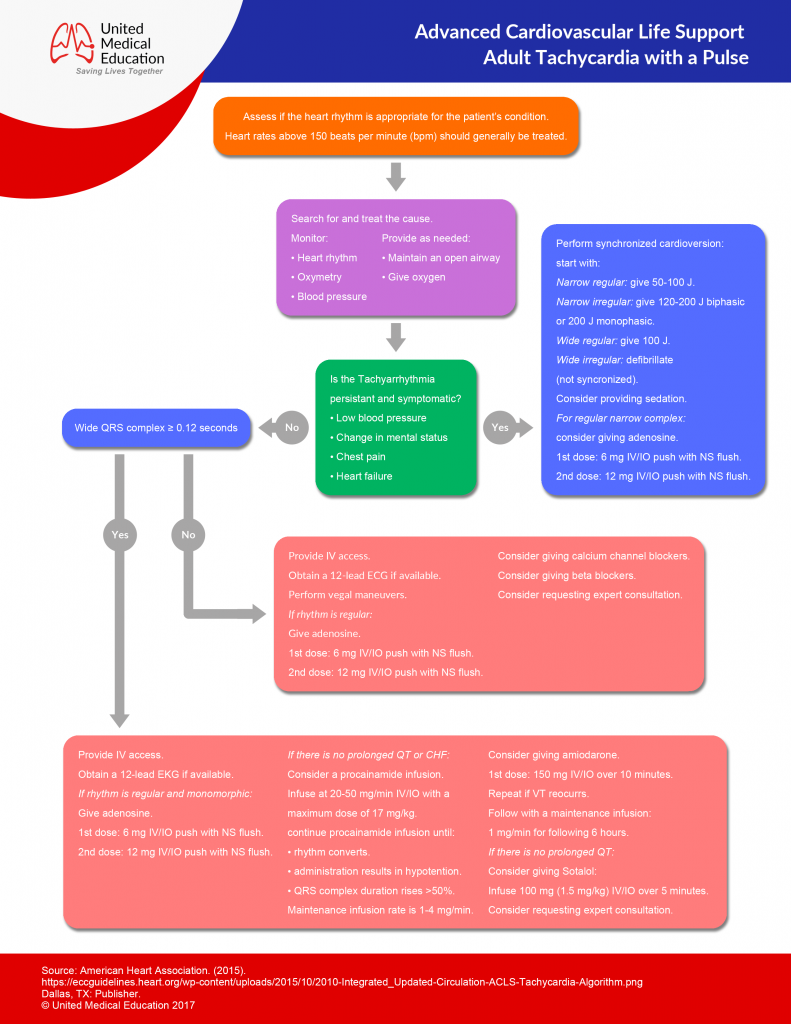
- Determine if the patient is Stable or Unstable.
- Initiate CABD and Secondary ABCD.
Narrow QRS Complex – Stable
Regular:
- Attempt vagal maneuvers.
- first line Rx is: Adenosine 1st dose: 6mg IV then 2nd and 3rd doses: 12mg IV
- Other Rx options include: Diltiazem and Beta blockers
Irregular:
- Rx options include: Diltiazem and Beta blockers
Narrow QRS Complex – Unstable
- Sedate the patient and provide cardioversion.
- Tx Atrial Fibrillation: first shock 100-200j
- Tx Atrial flutter and SVT: first shock 50-100j
Wide Complex – Stable
Regular:
Ventricular Tachycardia (monomorphic):
- Sedate the patient and provide cardioversion.
- Amiodarone 150mg IV over 10 min every 3-5 min, with a max of 2.2g in a 24hrs period.
- Procainamide 20 to 50 mg/min IV until arrhythmia resolves, hypotension occurs, there is >50% increase in QRS duration, or the max dose of 17 mg/kg is reached (Maintenance infusion: 1 to 4 mg/min)
- Sotalol 1.5 mg/kg over 5 min
- Procainamide and sotalol should be avoided in patients with prolonged QT.
SupraVentricular Tachycardia (SVT) with Aberrancy:
- Adenosine 1st dose: 6mg IV then 2nd and 3rd doses: 12mg IV.
Irregular:
Atrial Fibrillation with Aberrancy:
- Rx options include: Cardizem, Beta Blockers
Atrial Fibrillation with Wolff Parkinson White (delta wave):
- Avoid!!!: adenosine, verapamil, cardizem, and digoxin.
- Give Amiodarone 150mg IV over 10 min
Toursades de Pointes:
- Give magnesium 1 to 2g IV over 2 min
Wide Complex – Unstable
Ventricular Tachycardia (VT) – monomorphic:
- If still partially conscious, sedate the patient.
- Attempt to cardiovert: 1st attempt with 100j, 2nd attempt with 200j, 3rd attempt with 300j, then following attempts with 360j
Ventricular Tachycardia (VT) – polymorphic:
- Defibrilate the patient at 360j with a monophasic or 120-200j with a biphasic
Pulseless Ventricular Tachycardia / Ventricular Fibrillation (Refractory):
CABD, ABCD
Using defibrillator:
- Verify presence of VF: Defibrillate the patient at 360j using monophasic or at the factory recommended joules for a biphasic.
Drug treatment options:
- Epinephrine 1mg IV every 3-5min.
- Amiodarone 300mg IVP, repeated once in 3-5 min with following boluses at 150mg.
- Magnesium Sulfate: give 1-2gm in 1-2 min
Treat the cause of the arrhythmia.
Bradycardia (Rate < 60)
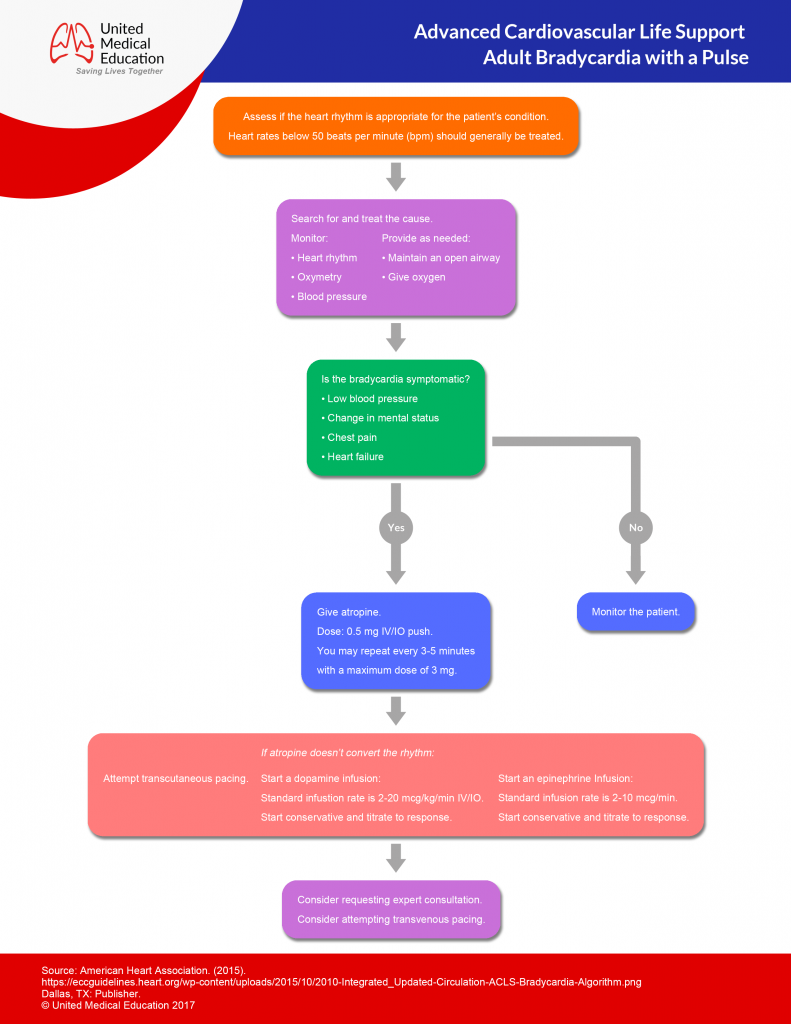
- CABD, ABCD
- Determine if the patient is stable or unstable.
Stable:
- Monitor for changes in the hemodynamic status of the patient.
Unstable:
- Give epinephrine 1mg IV every 3-5min until transcutaneous pacing can be initiated.
- Initiate transcutaneous pacing until transvenous pacing can be initiated.
- If TCP fails or intravenous pacing is delayed consider Epinephrine (2-10 mcg/min IV), Dopamine (5-20 mcg/kg/min), or Isoproterenol (3-20 mcg/mim).
- Treat causes (atropine 0.5-1mg IV may be used if vagal mechanism is suspected).
Asystole
- CABD, ABCD
- (if lead II is asystolic, confirm rhythm in leads avL and III.)
Drug therapy:
- Give epinephrine 1mg IV every 3-5min.
- Give atropine 1mg IV every 3-5 min, with a max dose of 3mg.
Pulseless Electrical Activity
- CABD, ABCD
Drug Therapy:
- Give epinephrine 1mg IV every 3-5min.
- Give Atropine if bradycardic arrhythmia is present: 1mg IV every 3-5 min with a max of 3mg.
- Treat the cause of the arrhythmia.
Acute Stroke
Initiated treatment within 10 min of arrival to the ER:
- CABD, ABCD
- Assess patient’s rhythm and treat with appropriate ACLS algorithm.
- Attempt to eliminate other causes of symptoms (use patient history).
- Obtain neurological assessment and tests by a specialist.
Initiated treatment within 25 min of arrival to the ER:
- Establish if onset of symptoms has been less than 3 hours.
- Continue neurological exams (non-Contrast CT scan), and monitor hemodynamics.
- Determine if fibrinolytic therapy is appropriate.
ACLS Case Scenarios
1) You are shopping at a grocery store and an elderly lady in the produce section suddenly grimaces, grabs her chest, and falls to the floor. You and a few others hurry to her side and she quickly becomes unresponsive.
Appropriate Action:
- Initiate CABD.
- Have one onlooker call for help.
- Have another onlooker retrieve the AED.
- Look, listen, and feel for breathing.
[Patient is not breathing.]
- Assess for pulse.
[Patient has no pulse.]
- Begin 2 person CPR.
[Have the student explain the steps of 2 person CPR.]
[Onlooker arrives with the AED.]
- Initiate appropriate use of the AED.
[Have the student explain the correct use of the AED.]
[After the AED analyzes the patient a shock is recommended.]
- Assure onlookers and yourself are clear of the patient.
- Initiate shock.
- Follow instructions of the AED until the arrival of medical transport.
2) You are just returning from lunch to the ER and you hear a code blue being initiated in bay 2. You run to the bay to find a patient confused, obtunded, and lethargic in the bed. Oxygen by NC, ECG, and IV access are already established. The nurse is unable to cycle a blood pressure. When assessing the ECG you see:

What should you do next?
- Initiate CABD and ABCD.
[Patient is breathing.]
[Faint pulse is felt approximately 35 times a minute.]
- Initiate transcutaneous pacing.
[Central line access is established.]
- Initiate transvenous pacing.
3) You enter your friends house to find their elderly grandmother staring at the wall and leaning to their side.
[Have student identify signs of stroke.]
[Have student perform prehospital stroke assessment.]
- Assess for unusual speech.
- Assess for facial drooping.
- Assess for arm drift.
- Attempt to establish a history of onset and events.
- Transport patient to hospital.
- Check patient’s blood glucose.
[Have student explain appropriate medical interventions for this patient.]
Congratulations!
You’re Ready to Certify.
Register for ACLS Certification
$119
Register for ACLS Recertificaiton
$119
